A Deep Dive into Hypospadias: What You Need to Know
Understanding Hypospadias: Anatomy and Diagnosis
Hypospadias is a congenital condition characterized by an abnormal opening of the urethra on the penis. Instead of being located at the tip, where it is typically found, the urethral opening may be found on the underside of the penis, varying in position from near the base to the head. The severity of hypospadias depends on the location of this opening along the shaft of the penis, which may also involve associated complications such as chordee, where the penis curves downwards because of fibrous tissue. Recognizing hypospadias typically involves a physical examination at birth, supported by imaging tests if further assessment is warranted. Pediatric urologists or surgeons specializing in genital conditions often make the diagnosis, providing the first avenue for parental inquiries and education about the condition.
Prevalence and Impact: Who Is Affected?
Hypospadias occurs in approximately 1 in every 125 to 250 male births, making it one of the most common congenital disorders affecting the male genitalia. The condition does not discriminate and can affect any race or demographic, although some studies suggest a slightly higher prevalence in individuals of Caucasian descent. The impact of hypospadias can extend beyond the physical aspects; it can influence social interactions, self-esteem, and personal identity as males grow and develop. Parents may feel stress or worry during the early years as they navigate medical consultations, and education about the condition. Understanding that early intervention and surgical correction can significantly improve quality of life underscores the need for awareness and action.
Mythbusting: Debunking Common Misconceptions
There are various myths surrounding hypospadias that can complicate the perception of this condition. One prevalent misconception is that hypospadias is the result of parental negligence or environmental factors easily controlled, which is not true as the exact cause remains unclear. Another myth is that all cases of hypospadias necessitate surgical intervention, when in fact the need for surgery is determined on a case-by-case basis, often based on the severity of the condition. Furthermore, some believe that hypospadias surgeries can completely erase all function issues or aesthetic concerns, while realistic expectations should be set, as this is more complex. Unpacking these misconceptions is essential in fostering informed decisions and reducing stigma surrounding the condition.
Cosmetic Surgery Options: Transformative Procedures Explained
From Consultation to Recovery: Navigating the Cosmetic Surgery Journey
The journey to cosmetic surgery for hypospadias begins with an in-depth consultation with a qualified urologist or pediatric surgeon experienced in this field. Here, families will discuss the specific type and degree of hypospadias, any associated conditions, potential complications, and the surgical techniques available. Emphasis is placed on setting realistic goals, where surgeons explain potential outcomes and limitations. Following the procedure, recovery is a crucial phase that demands attention. Post-operative care includes pain management, hygiene protocols, and follow-up appointments to monitor healing. It is vital for parents and children, through age-appropriate explanations, to understand that recovery can take several weeks, with particular care suggested during this time. This newfound knowledge prepares families for hurdles but also builds hope around the transformative potential of surgery.
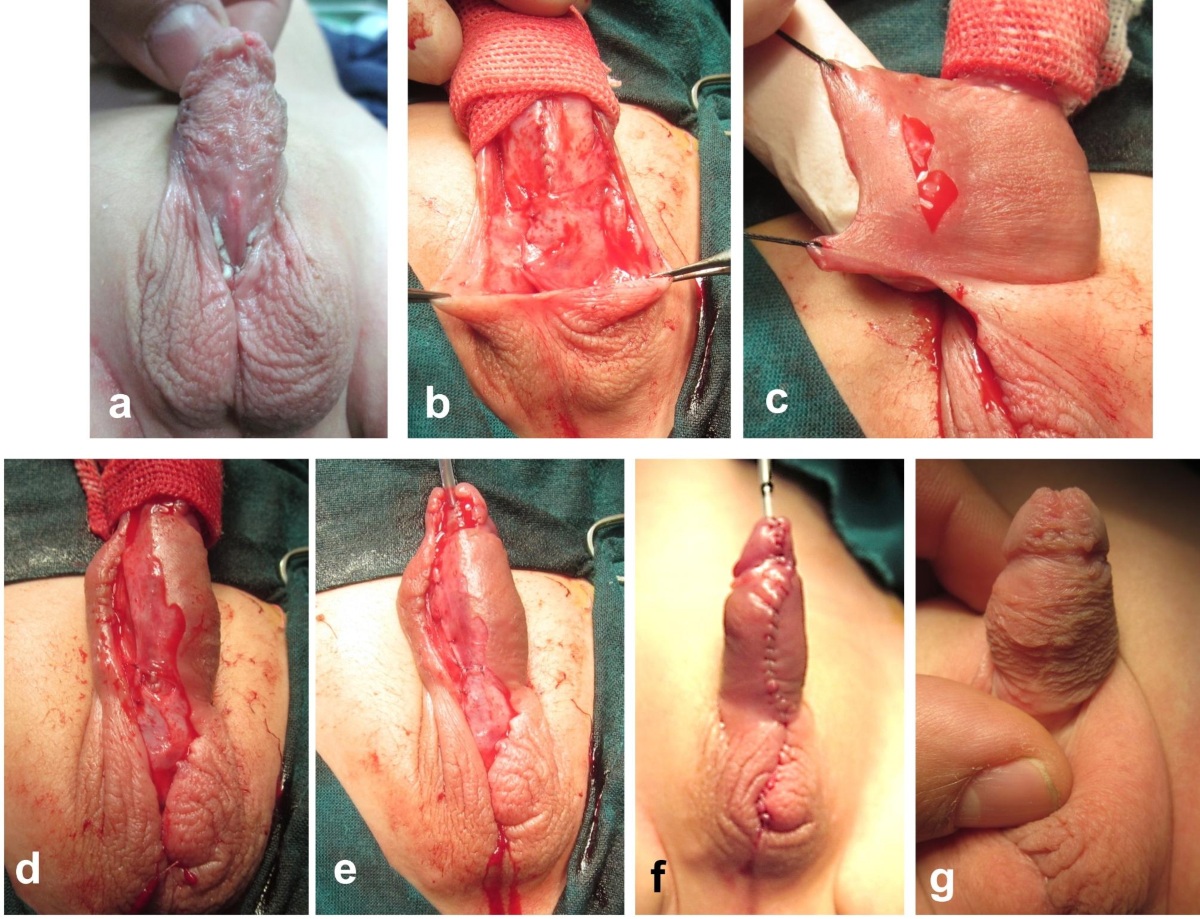
Types of Surgical Techniques: Choosing the Right Approach
There are several surgical techniques employed in combating hypospadias, with the choice largely dependent on the specific case of the individual patient. One of the most common methods is the TIP (Tubularized Incised Plate) technique, which has gained popularity for its efficacy and simplicity. In this approach, the existing urethral opening is reconstructed using existing tissue, which minimizes additional scarring and utilizes the body’s own materials for repair. Other techniques may include the Mathieu procedure, where a flap of skin is used to create a new urethra, or the staging repair, which might be necessary in more severe cases where surgeries are performed in intervals to allow proper healing. The choice of technique should consider various factors such as the age of the child, the extent of hypospadias, and the presence of any other complications that need to be addressed. By clearly communicating these options, families can engage meaningfully in medical decisions that affect their child’s well-being.
Realistic Expectations: Results and Risks of Surgery
It is essential for families to understand the balance of anticipation and pragmatism when considering hypospadias surgery. While surgical interventions have high success rates, yielding improved urinary function and aesthetic outcomes, they are not without risks. Potential complications can include urinary issues, need for additional surgeries, or dissatisfaction with aesthetic results. Parents need to communicate openly with medical professionals about the possibility of these outcomes, ensuring that emotional and psychological support systems are in place for both the child and family. Realistic expectations should encompass understanding that while surgery can significantly improve quality of life, it does not come with guarantees, and early intervention is not only about correction but promoting a healthy transition to adulthood.
The Emotional and Psychological Aspects of Hypospadias Surgery
The Impact on Self-Esteem: A Personal Journey
As children grow, the psychological implications of hypospadias extend far beyond physical appearance. The feelings of difference can contribute to self-esteem issues, particularly during pivotal developmental stages. The awareness of one’s body and associated anomalies can lead to identity challenges and social anxiety. Anecdotal evidence from personal journeys highlights that surgeries often offer significant relief and a sense of normalcy for those affected. However, not all children may have the same experience, making it crucial for families to monitor emotional responses and provide supportive environments that validate these feelings. Open dialogue about body image can assist children in articulating their experiences, facilitating healthier mental capacities to face challenges and foster resilience.
Parental Perspectives: Supporting Your Child Through Surgery
Parents play a pivotal role not just in the logistical aspects of managing a condition like hypospadias but also in the emotional support they afford their children. Many parents grapple with feelings of guilt or helplessness, yet it is essential to approach these situations with understanding and positivity. Supporting a child through surgery means being present physically, emotionally, and socially. Engaging children in discussions about their bodies can encourage empowerment, transforming what often feels like a stigma into a point of strength. Parent support groups can also be an invaluable resource, as they provide community insights, practical advice, and experience-sharing that can further aid in navigating this journey. It is vital for parents to maintain an optimistic outlook, which can positively influence their child’s perspective as they approach surgery.
Coping Mechanisms: Therapy and Community Support
Coping with the implications of hypospadias surgery is a multifaceted process that may benefit substantially from professional support. Counseling can be a crucial resource for children experiencing anxiety around surgery and self-image, and can assist in addressing trauma related to the unexpected aspects of the condition. Group therapies and community support organizations also offer a platform for individuals and families to connect with others sharing similar experiences. Many children thrive through these conversations where they can share stories, fears, and victories, eliminating feelings of isolation. Additionally, coping mechanisms focusing on mindfulness, stress management techniques, and artistic expression can provide emotional outlets for children and their families as they process their experiences in safe and nurturing environments.
Post-Op Life: What to Anticipate After Surgery
Care and Recovery: The Essential Guide
After hypospadias surgery, proper care is paramount to ensure a smooth recovery process. Parents are often handed a recovery plan that includes pain management strategies, rigid hygiene practices, and regular check-ins with healthcare providers. Children may experience discomfort post-surgery, which is manageable with prescribed pain relief; understanding this is crucial in normalizing their experience and promoting their comfort. It is also vital to educate parents on observing signs of complications, such as unusual swelling or signs of infection. Rest is critical during this period, offering a conducive environment for healing. Discipline regarding follow-up visits allows healthcare providers to assess recovery progress and bid an appropriate transition into normal activities.
Long-Term Outcomes: What Research Says
The long-term outcomes of cosmetic surgery for hypospadias are generally favorable, with high satisfaction rates reported among patients and their families. Research indicates that most well-executed surgical corrections lead not only to improved function but also to enhanced psychological well-being over time. While individual experiences may vary, studies highlight that patients often report significant improvements in self-esteem and social integration as they transition into adolescence and adulthood. Continuous follow-up examinations help ensure that any emerging issues are addressed promptly, contributing to an ongoing assessment of quality of life post-surgery. Parents and children should remain proactive about health, leveraging medical advancements to sustain a trajectory of well-being.
Finding Support: Resources for Families and Patients
The journey through hypospadias treatment and recovery can be markedly eased by tapping into a rich variety of resources available to families. Support organizations like the American Urological Association provide extensive information on hypospadias and connect families to local support networks. Online forums and community groups dedicated to urological conditions allow shared experiences and resources, serving as invaluable refuges for emotional and practical support. Parents can access literature that explores medical, emotional, and psychological dimensions of dealing with hypospadias, allowing them to feel equipped with knowledge and confidence. As the field of urology grows, so does the landscape of supportive resources, guaranteeing that families never feel alone in their journey toward understanding and overcoming hypospadias.